Connect With Us
Featured Articles
Items filtered by date: June 2022
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Heel Pain Can Indicate Plantar Fasciitis

There is no mistaking heel pain when it happens. It can be a gradual occurrence, and many people ignore the first pangs of heel pain. A common reason people experience heel pain is from a condition known as plantar fasciitis. It affects the plantar fascia, which is located on the sole of the foot and connects the heel to the toes. This band of tissue can become inflamed for several reasons, including wearing shoes that do not fit correctly and standing on hard surfaces for most of the day. Heel pain, often the first symptom of plantar fasciitis, can become severe if not treated promptly. Patients have found mild relief when the affected foot is elevated because pressure on the heel is reduced. There are specific stretches that can help the pain of plantar fasciitis. An effective stretch is done by standing on a step, followed by lowering the heels one at a time until a gentle stretch is felt. If you have with heel pain and think it may be caused by plantar fasciitis, it is strongly suggested that you speak with a podiatrist as quickly as possible so the correct treatment can promptly begin.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Foot & Ankle Associates of Maine. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Does It Feel Like There Is a Pebble in the Front of Your Shoe?
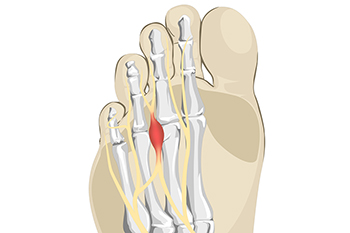
Intermetatarsal neuroma, or Morton’s neuroma, refers to a thickening of nerve tissue surrounding a nerve in the foot that is compressed or irritated. This compression can be the result of wearing high heels or other shoes that force the toes unnaturally into a narrow space. Morton’s neuroma typically occurs between the third and fourth toes. Engaging in certain athletic activities, like court sports or running, can also cause repetitive irritation to the nerves between the toes. Symptoms of Morton’s neuroma include pain, or the sensation of something being under the ball of the foot. There may be numbness, burning, or tingling, or it may feel like there is a bunched up sock or pebble in the front of the shoe. As the neuroma progresses over time, the pain may worsen and permanent nerve damage may occur. That is why it is very important to have your foot examined by a podiatrist if you believe you may have Morton’s neuroma. The earlier the diagnosis, the more likely it is that your podiatrist can treat the issue conservatively, rather than surgically.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Foot & Ankle Associates of Maine. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Let the Expert Treat Your Ingrown Toenails
Causes, Symptoms, and Treatment of Poor Blood Circulation in the Feet
Poor blood circulation in the feet and legs is often caused by peripheral artery disease (PAD), which is usually the result of a buildup of plaque in the arteries. Plaque buildup, or atherosclerosis, can be the result of excess calcium and cholesterol in the bloodstream. This restricts how much blood can flow through arteries. Reduced blood flow to a certain area of the body severely limits the amount of oxygen and nutrients that part of the body receives. This leads to degeneration in the muscles and other tissues. Sometimes, poor blood circulation in the feet and legs can be caused by other conditions, such as the damaging or inflammation of blood vessels, known as vasculitis.
The lack of oxygen and nutrients caused by poor blood circulation can restrict muscle growth and development, as well as cause muscle pain and cramps, weakness, and stiffness. Other common symptoms include numbness in the legs and feet, skin discoloration in the affected limbs, slower nail and hair growth, and erectile dysfunction in men. In more severe cases of PAD, pain can be present even when a person isn't exercising, and may range from mildly uncomfortable to completely debilitating.
Poor blood circulation in the feet and legs is more common in those who are overweight or obese, have diabetes, high blood pressure, high cholesterol, who smoke, or who have a family history of PAD or related conditions such as a heart attack, stroke, etc. Diabetes and smoking place a person at greatest risk for developing poor blood circulation, although advanced age, over 50, can also increase risk.
If you are experiencing poor blood circulation in the feet and legs caused by PAD, it is important to make changes to your lifestyle in order to reduce your risk of experiencing a heart attack or stroke caused by this condition. If you smoke, quit completely. This will increase the amount of oxygen in your bloodstream. Exercising and reducing the saturated fats in your diet. Saturated fats come from fatty meats, fried foods, whole milk, etc., can make a difference in improving blood circulation in feet. It is also important to avoid developing influenza and to carefully control your blood sugar if you have diabetes.
Your doctor may recommend combining lifestyle changes with a prescription medication regimen to improve blood circulation. The most commonly-used medications for PAD are called statins and work by blocking the amount of enzymes in your body that produce cholesterol. They are known by the brand names Zocor, Lipitor, Crestor, and others.
Signs of Poor Circulation

The circulatory system in the body is rarely thought about when it is working properly. Problems may occur when blood flow is restricted, and can cause reduced mobility, in addition to increasing the risk of a heart attack. A common cause of poor circulation is peripheral artery disease (PAD). One of the first signs of this condition can be pain in the feet and legs while walking, and this may be diminished by stretching and exercising at least three times per week. It is suggested to patients who smoke to stop or cut back, and people who are diabetic to control their sugar intake. A sign of poor circulation can include a wound on the foot that doesn't heal. Many people are unaware they may have cuts and scrapes on their feet as a result of the inability to feel sensations. Patients who are short of breath may be experiencing poor circulation, and this may be a subtle sign of a heart issue. If you have any of these symptoms, it is strongly suggested that you are under the care of a podiatrist who can offer you correct treatment options.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Foot & Ankle Associates of Maine. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
Rigid Versus Soft Orthotics

Custom orthotics are shoe or heel inserts prescribed by a doctor to help with various foot problems. Orthotics are used to correct foot deformities, help feet or ankles function better, and reduce risk of injury. Podiatrists can recommend custom orthotics as part of treatment plans for patients suffering from arthritis, bunions, flat feet or high arches, hammertoes, heel spurs, and plantar fasciitis. The type of material used for the orthotic determines how stiff it is. Rigid orthotics are usually made of a hard plastic or carbon fiber and provide more stability and support but may be less comfortable than softer orthotics. Softer orthotics are more flexible because they bend with your feet. Each type is appropriate for different foot conditions. Rigid orthotics are good for those who have plantar fasciitis or Achilles tendonitis. This type of orthotic takes more time to adjust to but over time becomes more comfortable. Soft orthotics are usually made of EVA (a more rubber-like material) and fit more closely against the foot than rigid orthotics. They are used for those who have heel pain as they mold to hurt areas and cushion sore spots. Soft orthotics are good for those who participate in high impact sports where the feet move quickly. Consulting with a podiatrist takes the decision of which type of orthotic is best for you out of your hands as they are experts in diagnosing foot problems and offering treatment options that fit your unique needs.
If you are having discomfort in your feet and would like to try orthotics, contact one of our podiatrists from Foot & Ankle Associates of Maine. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Brunswick, ME . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.